Credentialing | Verifying Trust, One Step At A Time!
In medical billing, credentialing is where the income begins. Without it, providers can not bill insurance, and payments are being delayed or denied. From verifying licenses to enrolling with payers, Credentialing in Medical Billing In The USA ensures providers are authorized, compliant, and ready to get reimbursed. Here is what you need to know to keep the income flowing.

Credentialing is a portion of the revenue cycle management process that verifies whether a service, healthcare provider, and company meet the criteria to deliver healthcare services to individuals. Credentialing in medical billing services is an essential process in RCM healthcare. The payers rely on the service deliverer to decide how much they reimburse the covered patients or clients.
Our expedited physician credentialing facilities work every file to payer standards, shorten the approval timelines, and maintain your credentialing in sync with the healthcare industry objectives. This way, you stay in touch, on schedule, and ahead.
No, redentialling is an ongoing procedure. Providers must regularly update their credentials, which involves renewing the license and upgrading the workings of their credentials. Maintaining current credentials confirms with insurance companies. It may also help update the working history and manage the malpractice insurance coverage.
There are types of medical credentialing, which involve:
The procedure of initial credentialing entails ensuring the credentials and the history of newly recruited healthcare professionals before they commence their practices.
Re-credentialing includes periodically verifying the background and qualifications of the healthcare professionals to confirm that their resumes meet industry standards.
Our enrollment officers have accomplished a 98% success rate of getting providers approved in premium payer networks with maximum privileges in their certain specialities. These method generally involves the following phases:
Our services process initiates with an in-depth survey conducted by our credentialing experts. This method includes comprehensive interviews with providers, collecting important data like license numbers, educational backgrounds, and professional history.
Our clinical credentialing facilities instruct providers in strategically selecting insurance partners aligned with their operational objectives and type of licenses. While also completing insurance panels depends on the practices' sites.
We take care of CAOH application submission, which controls doctor profiles, and maintain credentials current for smoother primary verification through the source. We also support you with healthcare payer enrollments, confirming quick insurance panel integrations, and exact profiles that improve network engagement.
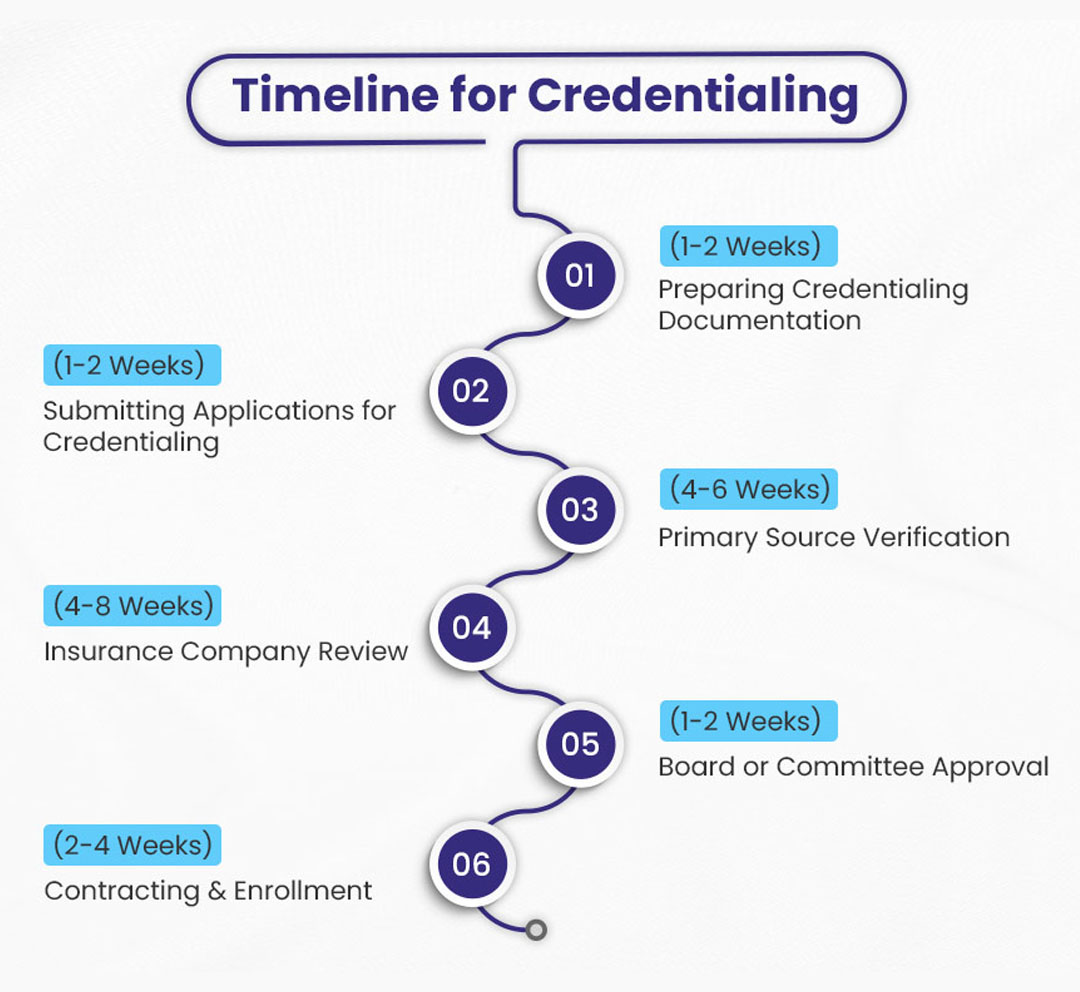
Although the general timeline is 60 to 120 days, our clinical credentialing experts take proactive steps to accelerate the methods. Our expert team engages in weekly interactions with payers, advocating fr quick processing and endorsement of applications.
Once the credentialing is completed, we instruct you about reviewing the fee schedules, eligibility CPT codes, and advocating for you if the panels are closed. Successful credentialing enables direct billing with preferable network rates.
We can help you in getting all the essential hospital privileges - admitting, the courtesy, or surgical, as credentialing concludes.
Our supportive team confirms your credentials to stay current with proactive tracking and daily reviews so you remain active and compliant without worry.
Here are some details about the comparison of standard and expedited credentialing:
| Aspects | Standard Credentialing | Expedited Credentialing |
|---|---|---|
| Main Objective | Daily processing of new provider applications. | Quick onboarding of providers when time is crucial. |
| Processing Duration | Generally, 60 to 120 days. | It can be done within 30 to 35 days. |
| Suitability | All providers | Restricted to some situations |
| Payer Participation | All payers adhere to scheduled credentialing. | Only some payers offer expedited credentialing. |
| Provisional Approval | Not available. | Sometimes it might permit the provider to initiate seeing the patient and billing. |
Elements of credentialing involve, but are not restricted to, these components, which are explained below:
Verification of education and Training:
Licensure Verification:
Board certification:
Work background review:
Privileging (For medical roles):
Malpractice record check out:
Here are some of the advantages of credentialing mentioned below:
Meeting credentialing standards confirms you have higher-quality care and compliance in medical care. Patients trust credentialed providers for a secure and better method.
Credentialing with payers secures timely reimbursement for facilities rendered. Without it, claims are riskier denials, which lead to loss of income.
The credentialing process permits the providers to accept more insurance plans, attracting a wider patient population. More individuals mean higher revenue opportunities.
Being credentialed elevates the credibility and trustworthiness with individuals. A strong reputation draws more clients looking for reliable care.
Understanding the credentialing method inside out and having a powerful connection with the payers aids you in getting credentialed quickly. The third-party credentialing facilities providers, such as DocVaz, have wide expertise and experience in credentialing process. They can support you in seamlessly completing the method and gain the maximum advantages.
Without credentialing, the providers cannot bill or get any reimbursement from insurance payers, and this might affect the circulation of cash or income.
It generally takes between 30 and 120 days, based on the payers and completeness of the applications.
All the healthcare providers who desire to bill insurance, including physicians, nurses, practitioners, therapists, and hospitals, should be credentialed.
Some usual documentation involves medical licenses, board certifications, malpractice insurance, and the complete profile of CAQH.
Credentialing typically needs to be updated every 2 to 3 years to manage the active status with your payers.
Claims might be denied, leading to delayed or lost payments ,and the providers might be excluded from your insurance connections.