Dealing with claim denials can be a time-consuming and frustrating process for healthcare providers.
Our denial management services are designed to assist hospitals and medical practices in improving
their clean-claims rate, efficiently managing denied claims, and providing expert support with appeals.
By partnering with DocVaz, you’ll get the help you need to handle denials swiftly and effectively.
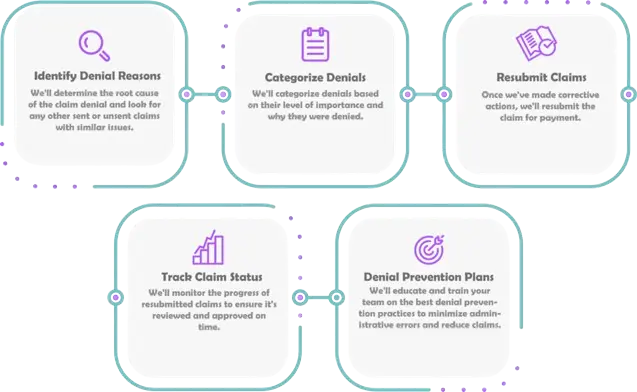
Claim denials can negatively impact your practice’s cash flow and overall efficiency. With DocVaz, our denial management services focus on identifying the root causes of denials and implementing strategies to prevent them. This ensures smoother claim submission processes and increased revenue recovery for your practice.
Struggling with denied claims? Our medical billing services can help turn things around. Here’s how our denial management solutions benefit your practice:
More Clean Claims, Less Hassle: Our process addresses the root causes of denials, leading to fewer rejected claims and more revenue. We implement preventive measures to significantly increase your clean claim rate.
Maximized Reimbursements, Fewer Headaches: With our denial management solutions, you’ll receive the reimbursement you deserve by addressing denials quickly, capturing lost revenue, and reducing frustration.
Improved Patient Experience: Claim denials can affect patient satisfaction. By reducing delays and denials, we help create a smoother billing experience, promoting loyalty and trust with your patients.
Streamlined Operations, Reduced Costs: We optimize your claim submission process, reducing the administrative burden and freeing up your staff for more important tasks. Our efficient handling of denials saves you time and resources.
Stay Compliant and Future-Ready: Our team stays up-to-date on the latest payer guidelines, coding standards, and denial prevention techniques, keeping your practice compliant and ready for future challenges.
By partnering with a medical billing service like DocVaz, you can focus on providing exceptional patient care while we handle the complexities of denial management and medical billing.




At DocVaz, we understand the importance of denial management in medical billing. Our goal is to help healthcare providers focus on what matters most—providing quality care—while we take care of the billing headaches.
Our team stays informed on the latest updates in the healthcare industry. We perform thorough analyses of your claims to identify patterns and reasons behind denials.
We evaluate denials based on factors like claim age, adherence to deadlines, and other compliance guidelines, ensuring that each claim is accurately assessed and resolved quickly.
A claim denial occurs when an insurance company refuses to pay for a service provided. This usually happens when the service isn’t covered or doesn’t meet the company’s requirements.
Preventing denials starts with accurate coding, complete claim submissions, and timely authorizations. Our denial management services ensure all claims are submitted correctly, minimizing the chances of rejection.
If your claim gets denied, we’ll help you understand the reason behind the denial and assist you in filing an appeal if necessary. With our denial management services, you can be confident that every claim will be handled with care.